Case Of The Month
October 2016
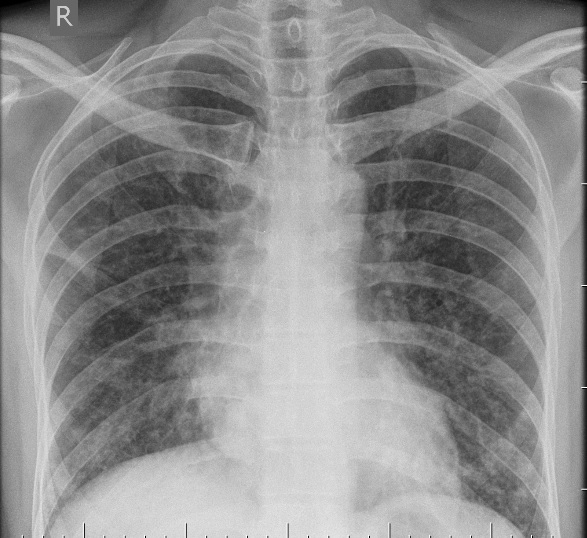
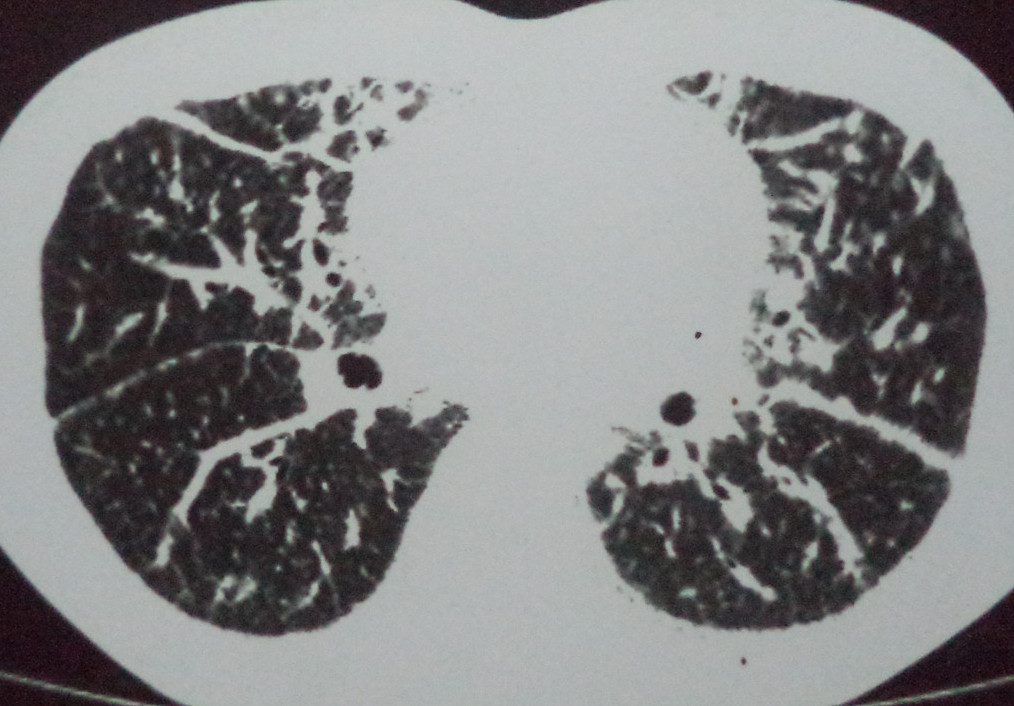
15 year old boy presented with exertional dyspnoea & persistent cough since childhood. The patient had clubbing. Pectus excavatum was present. Coarse crepitations and rhonchi were heard bilaterally over all areas. Sputum AFB came out to be negative and Sputum cytology was inconclusive. Blood Routine Examination , Urine Routine Examination,Random Blood Sugar, Renal Function Tests, Serum Electrolytes including Serum calcium and phosphorus and Serum LDH were within normal limits. 6 Minute Walk Test was done. There was no desaturation. Spiromerty showed evidence of obstructive lung disease. CXR and CT images of the patient are given below. What are the differential diagnosis?
Previous Case
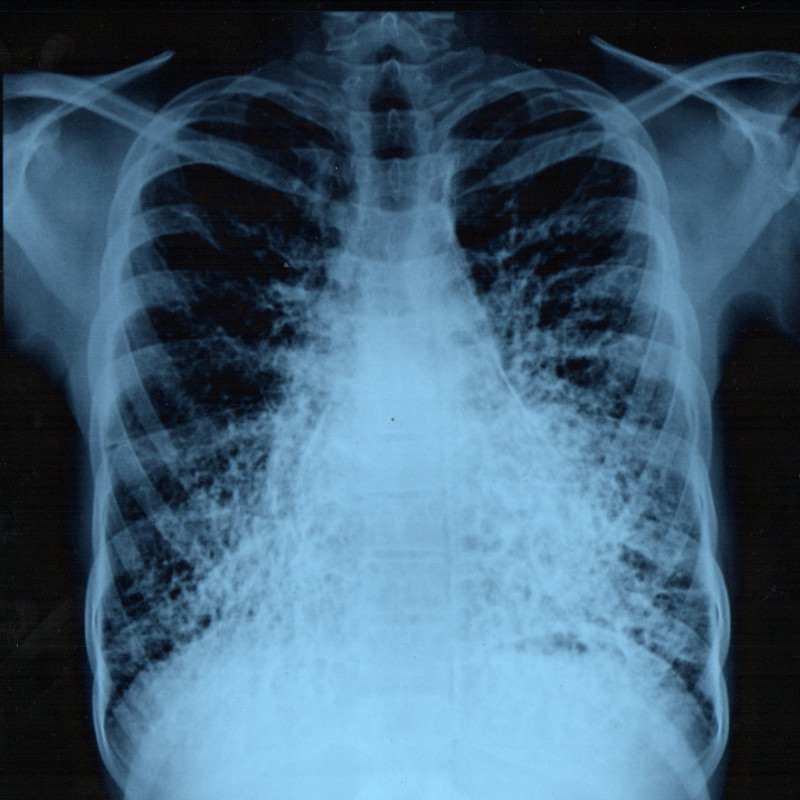
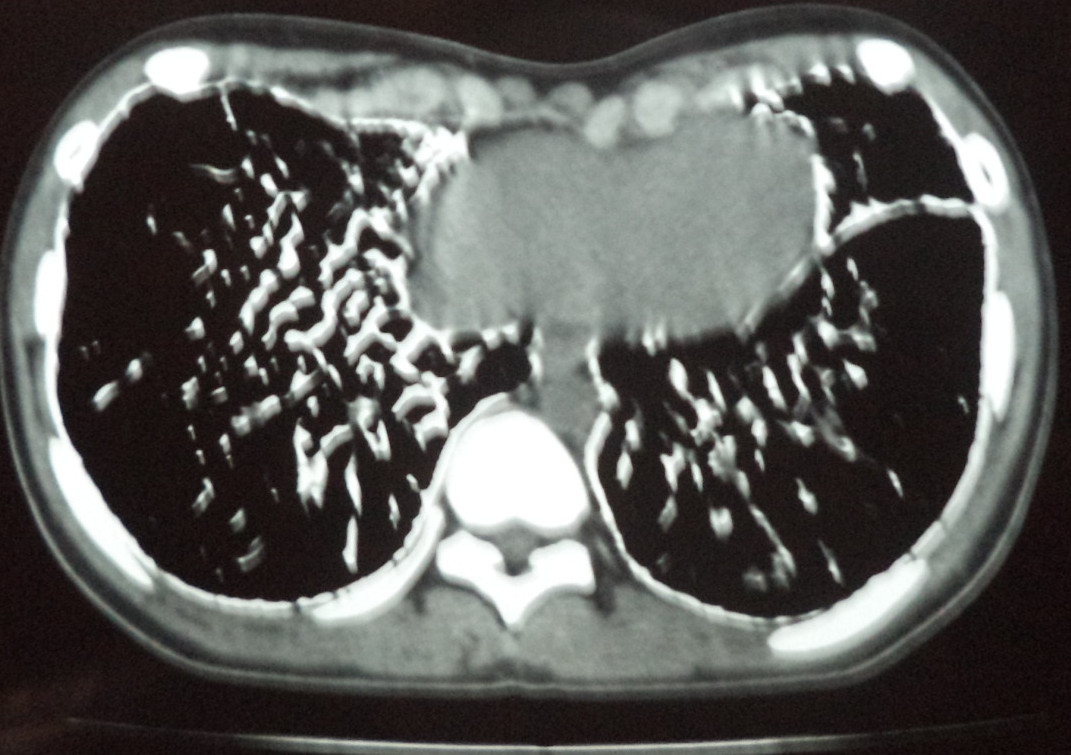
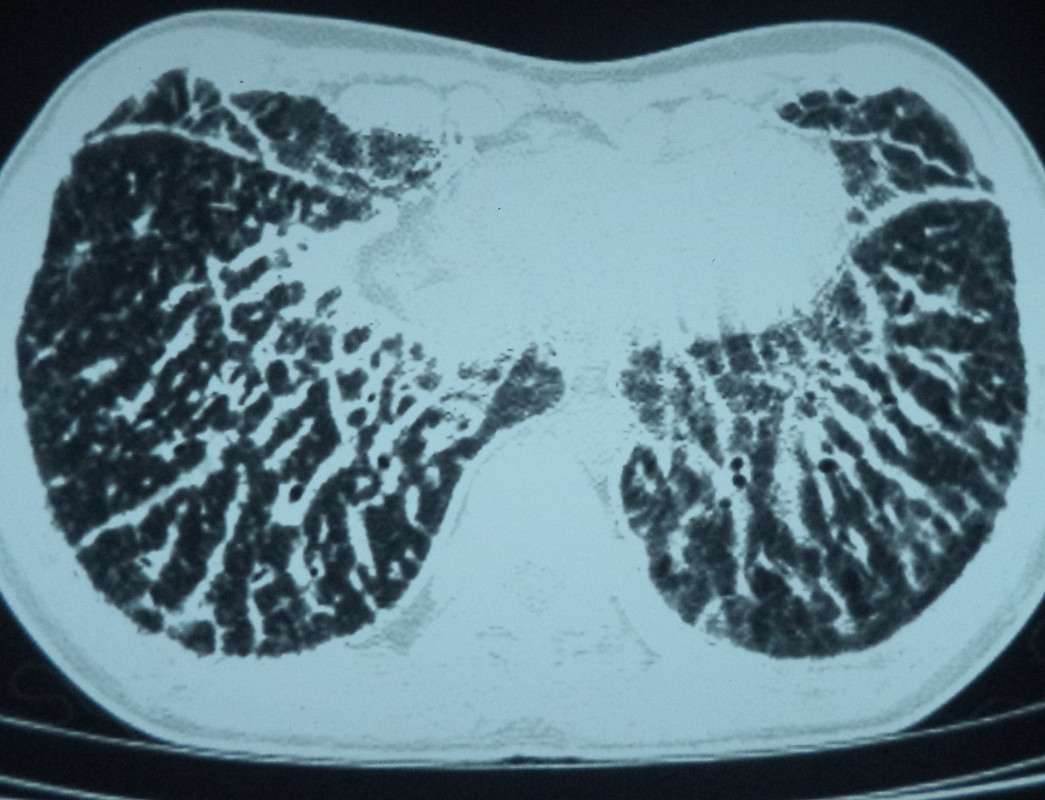
42 year old gentleman with no known comorbidities presented with 4 months history of shortness of breath which was insidious in onset and slowly progressive. He was a clerk by profession and had no atopic background. He denied any occupational exposure to dust, fumes or chemical agents. There were no pet animals or birds at home. There was no orthopnea or wheeze. There was dry cough which was much bearable as per his own words. There was no fever, swelling of feet, chest pain or palpitation. There was loss of weight of 4 kg over 4 months. Physical evaluation revealed a slightly uncomfortable gentleman with a respiratory rate of 28 per minute, heart rate of 104 per minute and oxygen saturation of 92% on room air. The neck was supple without venous engorgement. Chest examination revealed bilateral fine crackles audible over all lung areas. Chest radiograph is shown above. Echocardiography revealed normal left ventricular systolic function as well as heart valves with features of mild PAH. Representative images of CT chest (lung window – HR cuts) are depicted.
What are the differentials? How should the clinician proceed?
Answer :
HIV infection (WHO – clinical stage 4) with pneumocystis pneumonia
Discussion
The subject had subacute onset and progression of dyspnea and weight loss. The onset of the disease, radiological pattern, and profound hypoxia suggested possible pneumocystis pneumonia. The differentials entertained included interstitial / cystic lung diseases of varying etiology, bacterial infectious pneumonias, fungal pneumonias and connective tissue diseases. He denied any high risk sexual behavior or history of blood transfusions / needle stick injury. Despite this, HIV antibody testing done by ELISA turned out to be positive. Western Blot test re-inforced the disease status. Induced sputum examination confirmed the diagnosis of pneumocystis. He was treated with high dose cotrimoxazole as well as broad spectrum antibiotics, but developed clinical worsening with bilateral pneumothoraces, large air leak, sepsis and multiorgan failure. He finally succumbed to his illness.
The HRCT images in this case exhibit upper lobe small cystic parenchymal lesions with ground glassing, and focal crazy paving appearance. The differential diagnosis of cystic lung disease include Langerhans cell histiocytosis, cystic sarcoidosis, chronic hypersensitivity pneumonitis, pneumoconiosis, mycobacterial disease, septic emboli and in ladies lymphangioleiomyomatosis(1). Of these, PCP, sarcoidosis, chronic HP and some pneumoconiosis produce upper lobe predominant cystic disease. The cysts of LCH also tend to be upper and mid zone predominant. PCP can have upper lobe cystic disease with ground glassing, reticulation and focal crazy paving appearance.
The “crazy-paving” pattern in HRCT refers to scattered or diffuse ground-glass attenuation with superimposed interlobular septal thickening and intralobular lines(2). Once thought to be pathognomonic of pulmonary alveolar proteinosis, it is now recognized that many diseases can present with this radiological finding.This differentials of crazy paving pattern include infectious, neoplastic, idiopathic, inhalational, and sanguineous disorders. Specific disorders that can cause the crazy-paving pattern include Pneumocystis carinii pneumonia, mucinous bronchioloalveolar carcinoma, pulmonary alveolar proteinosis, sarcoidosis, nonspecific interstitial pneumonia, organizing pneumonia, exogenous lipoid pneumonia, adult respiratory distress syndrome, and pulmonary hemorrhage syndromes.
Although the chest radiograph in early clinical PCP can be normal in a small subset of patients, HRCT almost always reveals demonstrable abnormalities. Widespread ground glass opacities is the commonest abnormality described(3). Upper lobe prediclition has been described. With more advanced disease, septal lines with or without intralobular lines superimposed on ground-glass opacity (crazy paving pattern) and consolidation may develop(4). Pulmonary cysts of varying shape, size, and wall thickness occur in as many as one third of patients with PCP(5). Cysts are associated with an increased frequency of spontaneous pneumothorax. Non-HIV infected patients with PCP tend to have greater ground glassing, more consolidation, lesser cystic changes, sometimes nodular with tree in bud shadows and more rapid radiological progression. This has been ascribed to increased host inflammatory response in non-HIV infected individuals. Very rarely, a chronic condition termed chronic PCP has been described with chronic interstitial fibrosis(6).
References
- Angelica F, Francisco F, Souza AS et al. Multiple cystic lung disease. Eur Respir Rev 2015; 24: 552–64
- Rossi SE, Erasmus JJ, Volpachio M, et al. Crazy paving pattern at thin section CT of the lungs: Radiologic-pathologic overview. Radio Graphics 2003; 23: 1509-19
- Kanne JP, Yandow DR, Meyer CA. Pneumocystic jirovecii pneumonia: HRCT findings in patients with and without HIV infection. AJR 2012; 198: W 555-W 561
- Fujii T, Nakamura T, Iwamoto A. Pneumocystis pneumonia in patients with HIV infection: clinical manifestations, laboratory findings, and radiological features. J Infect Chemother 2007; 13:1–7
- Boiselle PM, Crans CA Jr, Kaplan MA. The changing face of Pneumocystis carinii pneumonia in AIDS patients. AJR 1999; 172:1301–1309
- Wassermann K, Pothoff G, Kirn E, Fatkenheuer G, Krueger GR. Chronic Pneumocystis carinii pneumonia in AIDS. Chest 1993; 104:667–672
Case contributed by – Department of Pulmonary Medicine, Rajagiri Hospital, Aluva.
Download CaseWinners Names
Previous cases
Governing Council

Dr. Davis Paul C( President )

Dr. Sanjeev Nair( President Elect )

Dr. B. Jayaprakash( Vice President )

Dr. Judo Vachaparambil( Secretary )

Dr. Unni R Baby( Joint Secretary )

Dr. Vipin Varkey( Treasurer )

Dr. P. Venugopal( Editor Pulmon )


Send Your Answers